Engorgement Relief
Author Kelly Bonyata, BS, IBCLC - KellyMom

Reverse Pressure Softening (RPS) uses gentle positive pressure to soften a 1-2 inch area of the areola surrounding the base of the nipple, temporarily moving some swelling slightly backward and upward into the breast. RPS may be applied by the health care provider, and/or taught to the mother/significant others, if necessary, over the telephone.
Interstitial fluid volume increases 30% above normal before edema becomes visible (Guyton). To contain edema, areolar tissues must expand, limiting their ability to extend the nipple well into the baby’s mouth. Early proactive use of RPS causes no harm and may facilitate increased milk transfer, reduce risk of nipple trauma, and help resolve engorgement.
Conversely, pumping may attract edema into the flange area, especially at maximum vacuum settings. Areolar tissue may then appear “thickened”, seeming to “bury” the subareolar ducts. Then, neither infant tongue action, fingertip expression nor the pump itself removes milk very successfully.
RPS is best performed immediately before each attempt to latch, for as many feedings as needed:
- The mother may prefer to apply RPS herself, or the HCP, with her permission, may apply RPS.
- facing the mother, or
- from slightly behind the mother, reaching over her shoulders
- or place his/her fingers over those of the mother, to reinforce pressure.
- The firmer or more swollen the areola, the more time is needed to achieve pliability.
- RPS often forms temporary “dimples” or “pits”, but edema soon re-enters the pits after pressure is released.
- Positioning the mother with severe edema flat on her back during RPS delays re-entry of swelling, allowing a longer window of time for latching.
- Firmly but gently, press steadily on the areola, right at the nipple base.
- Pressure should not be firm enough to cause pain. Avoid discomfort with less pressure for longer intervals.
- Press inward toward the chest wall for a full 60 seconds or longer (10-20 minutes or more if needed. This is a good time for instructions.)
- Any finger combination may be used. (See diagrams)
- Mothers may find short nails with curved fingertips of both hands the most effective method.
- One-handed methods are convenient if the other hand is busy.
- HCP’s may find straight-fingers or two-thumb methods more convenient.
- Use the flats of two thumbs or the first several fingers on each hand lengthwise above and below the nipple, creating a 1-2 inch long depression.
- Continue to alternate in opposite quadrants, with repeated 2 minute periods of pressure, partially overlapping the first set of pits, to keep edema displaced from the entire area at the base of the nipple.
- After RPS, additional fingertip expression to further soften the areola is much easier, more comfortable and more productive. Creating a special niche for the chin often permits deeper latching.
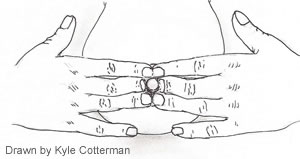
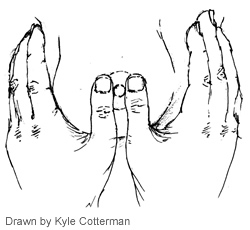
Two handed, one-step method
Fingernails short, fingertips curved;each one touching the side of nipple.
Two handed, two-step method
Using 2 or 3 straight fingers on each side, first knuckles touching nipple. Move ¼ turn. Repeat above & below nipple.
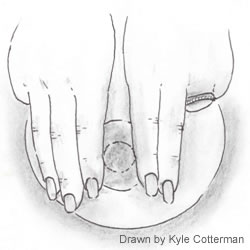
Two thumbs, two-step method (Step 1).
Using straight thumbs, base of thumbnail even with side of nipple.

Two thumbs, two-step method (Step 2).
Move ¼ turn. Repeat above & below nipple.

One handed “flower hold”
Fingernails short, fingertips curved, placed where baby’s tongue will go.
(To see your areola better, try using a hand mirror.)
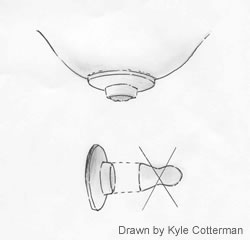
Soft ring method
Cut off bottom half of an artificial nipple to place on areola to press with fingers.
Benefits of RPS include:
- Steady stimulation of nerves under the areola automatically triggers the milk ejection reflex, propelling milk forward in the breast, nearly always within 1-2 minutes or less.
- Excess interstitial fluid is temporarily moved in the direction of natural lymphatic drainage.
- Displacing milk slightly backward into deeper ducts relieves over-distention of subareolar ducts, reducing latch discomfort and facilitating milk transfer.
- Areolar elasticity is freed for
- extending the nipple more deeply into baby’s mouth
- responding to the rippling of the tongue.
Thank you Kelly Bonyata, founder of KellyMom for giving me permission to reproduce and distribute this article. I'd like to credit Kyle Cotterman for the diagrams.
Guyton, AC, Basic Human Physiology: Normal Function and Mechanisms of Disease, 2nd Ed., W. B. Saunders Co. Philadelphia, 1977, p. 321.