Lactose intolerance or Lactose Overload

In my clinical practice I come across so many parents that say, ‘my baby is lactose intolerant’. But so often the baby is not. It’s not the parents fault – there’s so much information and confusion out there on lactose intolerance, and a lot of misinformation.
I wanted to help parents cut through the confusion and after receiving many queries about this following on from my blog ‘the why and why not of cluster feeding’, I felt it was time to deal with the buzz around lactose intolerance.
So, this post will define the differences between lactose intolerance and lactose overload; cover how both of these occur and what treatment is needed to make the baby more comfortable or stop it altogether.
What is lactose?
Let’s start at the beginning. Lactose is the sugar, carbohydrate, in all mammalian milks and it’s made up of two sugar molecules bound together – glucose and galactose.
Lactose naturally occurs in breast milk and dairy products such as milk and cheese. It can also be found in most formulas. Lactose is synthesised in the breast by milk making cells. You may be told that lactose is only in the foremilk, the first milk your baby drinks, but it is actually throughout the entire milk, but more concentrated in the fore milk because the hind milk has a higher fat content.
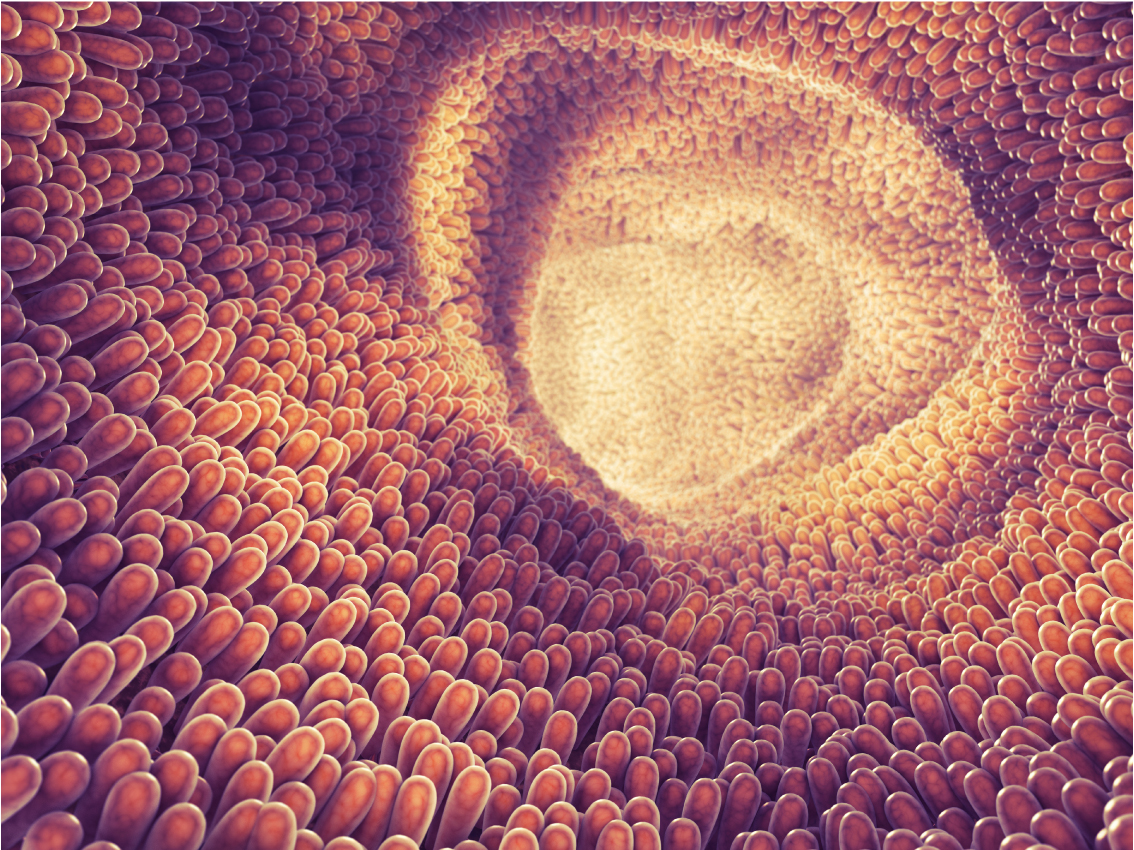
To digest lactose the body produces an enzyme called lactase, which breaks down the lactose. The lactase enzyme is made in the microvilli lining of the small intestine. These villi naturally recreate themselves, continually producing cells that make lactase, which then absorb the lactose as it passes through the digestive tract.
Article continued after free group coaching ticket
Why do we need lactose?
- Lactose helps babies to thrive by providing the calories they need to grow.
- Calcium and phosphorus aid bone development and lactose helps your child absorb these two essential minerals.
- Friendly bacteria are thought to develop because of lactose, giving newborns the ability to fight off unwanted bacteria, thus keeping the digestive system healthy.
- Healthy brain development and optimum growth of the nervous system is another vital function of lactose.
What is lactose intolerance (aka Congenital or developmental lactose intolerance)?
This is a very rare conditions that, according to the American Academy of Paediatrics, occurs when a mother and father pass on the same gene variant to their baby, thus providing baby with a lack of lactase enzyme. Alternatively, premature newborns can also have developmental lactose intolerance, but this only lasts for a short time after birth. If affected newborns are not given a lactose-free infant formula at this time, then they may develop severe dehydration and weight loss. This kind of lactose intolerance obviously requires medical and dietary interventions.
What is secondary lactose intolerance?
This happens when villi in the small intestine have been damaged either by gastroenteritis, or food sensitivities, such as gluten, thus effecting the production of the lactase enzyme. This means the lactose cannot be broken down appropriately.
Secondary intolerance is temporary since the villi are always creating more cells that produce lactase. So when the child’s gastro infection stops, or the possible food sensitivities are reduced or eliminated, lactose can again be absorbed correctly. So, if you know your child is well, doesn’t have true lactose intolerance (see the symptoms listed below) and you are doing everything right to avoid lactose overload (see the information for this below), then you can try eliminating gluten.
What is lactose overload?
This is what the majority of newborns actually have but is so often, wrongly labelled as lactose intolerance. Lactose Overload is caused by having too much lactose in the system for the baby to break down, so the digestive system carries on as it should, but it can’t cope with the amount of lactose it is receiving.
The overload of lactose then moves from the small intestine into the large intestine where it draws in more water through the intestinal wall – this is called osmosis. The bacteria present then ferments the lactose producing a range of symptoms that are listed below. When this happens the baby, or infant actually looks like they are trying to suck more. This is because sucking is their instinctual tool to enable comfort, and lactose overload obviously creates discomfort. However, this looking to suck (the rooting reflex) is often misread and mistaught as a hunger cue only, leading to parents feeding more, resulting in more overload of lactose to produce more symptoms. And so, the cycle goes.
Unfortunately, the widely taught practices of feeding from both breasts in one sitting, in quick succession, or cluster feeding creates lactose overload for our newborns, as does overfeeding. Not only because the amount of lactose the child receives is too much, but also because these feeding practices push the milk through the digestive tract too quickly, which doesn’t allow enough time for the lactose to be broken down appropriately.
Lactase drops are sometimes recommended as a treatment for secondary lactose and lactose overload but again, these are not necessary for treatment as we can heal both of these naturally. There is also some debate as to whether they are effective.
Symptom list and what you can do now to heal these is after Three Top Burping Tips free download.
3 Top Burping Tips
These three top tips may just surprise you for many parents around the world are taught to do these burping practices, but they actually hinder the release of trapped air in the stomach.

- Stimulating air release
- Recognise a wind-cue
- Beneficial positioning

WHAT'S INSIDE
- Stimulating air release
- Recognise a wind-cue
- Beneficial positioning
I see a lot of babies and infants in my clinical work that have lactose overload, and I now group these symptoms under the term Digestive Overload, since many of the Digestive Overload causes and symptoms overlap each other.
If all this sounds overwhelming, here’s the good news. Lactose overload, like secondary lactose intolerance, can be healed naturally by reassessing the child’s diet and changing feeding practices. These changes can bring remarkable results – and it’s something I regularly help parents do in my clinic.
Symptoms of secondary lactose intolerance or lactose overload
These two forms of lactose imbalance have the same symptoms.
- Irritability, grizzling, inconsolable crying, screaming.
- Bloating, intestinal cramps, excessive gas.
- Frequent watery, frothy and/or explosive bowel motions. Sometimes green in colour with an offensive odour. Stools are also acidic, effecting baby’s skin if left on the skin for too long.
- Wakefulness from discomfort with episodes of longer periods of sleep, but this is often from exhaustion through crying and lack of sleep rather than because they feel comfortable.
- Frequent searching for something to suck - exhibiting the ‘root reflex’.
- Weight gains that are consistently at the upper regions or beyond recommended levels, or, as described by Morris Wessel, your baby will ‘look to otherwise be thriving’.
- Arching backwards or sideways, writhing, wriggling.
- Pedalling legs.
- Gulping their food, seeming very hungry while being restless – sometimes refusing to feed, pulling off the nipple, or when bottle-fed, having flailing arms and legs with much turning of the head because of digestive discomfort.
What you can do to prevent lactose overload
- Breastfeed from one breast in one sitting
- Feed baby at intervals that work alongside their digestive function – every 3 ½ to 4 hours
- Feed your baby in accordance with their stomach capacity for each age
- Stop cluster feeding
- Take dairy out of the breastfeeding diet, or change from dairy formula to goat formula
- Learn the suck swallow ratio to help you reduce overfeeding while breastfeeding
- Have a 1:1 virtual consultation with me, especially since there are often other causes that creating Digestive Overload symptoms.
Please note:
Secondary lactose intolerance and lactose overload are not the same as dairy intolerance or dairy overload. In the latter two the child is actually reacting to the proteins in dairy, casein and whey. Not the lactose. This creates slightly different symptoms but again, these can be healed naturally.

 Submitting data
Submitting data