Reflux medication for baby

When a parent finds themselves walking down the medical path for gastroesophageal reflux (GER) there are standard explanations that one is told, and standard steps that are offered. In this article we delve into the standard medical pathway for reflux, and the effects of some of the prescribed potions. If you would like an overview of the symptoms of reflux and to read about the true causes, which I do recommend before reading this article, please go to this blog – what causes baby reflux? The information may surprise you.
Now it’s important to define that this article is talking about Gastroesophaguel Reflux (GER/GOR) not Gastroesophaguel Reflux Disease (GERD/GORD). If your baby is bringing up the majority of their milk after every feed and experiencing little to no weight gain then they may have GERD and medical assistance is needed. On the other hand, if baby is managing to retain the majority of their milk, having big to small posits throughout the day after each feed, while gaining steady weight (20-25grams a day for 0-6 month olds), perhaps very large weight gains even, then they have GER and this can be healed naturally. This is what I do within my work.
Also, for those parents who, on the recommendation of health professionals, have administered acid inhibitors to their newborns, this next bit of information may be upsetting. If you are one of these parents please remember this as you read; you understandably placed your faith in the hands of your health professional who probably thought they were doing the best they could for you. You have been the best parents possible by accepting a solution that has been advocated. I understand the desperation to find something that works, something that stops the crying, that reinstates some kind of sanity back into life, gifting you the newborn and life you envisioned. You did what any good parent would do. You tried something that might help and it seemed to because it brought calm.
Medical pathway for reflux
A very common scenario that I have families relay to me in clinic when they talk about the things they have tried to help their baby’s reflux is along these lines… “first we tried Gaviscon, but that only made her constipated and did nothing. Then the Paediatrician prescribed Ranitidine (H2 Blocker) and even though we didn’t want her on medication we thought we’d give it ago because nothing else was working. At first she seemed a little better, the reflux didn’t stop but she was calmer. But this only lasted for about a week-and-a-half, then she was screaming again. They then prescribed Omeprazole (Proton Pump Inhibitor) and we still haven’t seen a dramatic improvement. She’s been on it for a month now and they want to increase her dose but we aren’t that keen. We are at our wits, exhausted and just don’t know what else to do. It’s awful to watch her like this!”
Having held far too many newborns that are in pain, I very much know that doing so for parents is OH SO HARD and a HUGE EMOTIONAL ASK (words can’t describe it really). Both because of the overwhelming connection they feel to their baby but also, let’s face it, because of the non-connection that can start to take place from living with reflux every day with very little resolution or reprieve.

The advice that is largely given is that reflux symptoms are caused by acid moving up the oesophagus because of an immature digestive system, resulting in a lazy sphincter muscle at the bottom of the oesophagus allowing regurgitation of milk and acid. Therefore the medical pathway to so call remedy reflux symptoms is to stop acid moving up the oesophagus. To do this the medications below are prescribed in written order. Just to say here to, acid is actually a symptom from the cause of reflux, which is not a lazy sphincter muscle but Digestive Overload.
Prescribed medication
Gaviscon
Three ingredients make up Gaviscon – sodium alginate, sodium bicarbonate (baking soda) and calcium carbonate. Soduim alginate (E401) is made from seaweed and when this is in contact with liquid it forms a thick gel.1 When the sodium bicarbonate comes in contact with gastric acids it produces carbon dioxide bubbles that get trapped in the gel.1 These bubbles cause the thick gel to form a floating foam that sits on top of the stomach contents.1 The calcium carbonate then reacts with the soft foam, adding loft and tightening it up. The raft then slides up the oesophagus and creates a battier, which prevents acid in the stomach from pushing into the esophagus.1,2 The stomach acid is also neutralized somewhat by the carbonate and bicarbonate, which is said to be helpful to reduce the severity of the reflux symptoms and the frequent reflux episodes.1
However, given acid is not the cause of reflux, or the majority of reflux symptoms, albeit a bi-product of the causes for some newborns, one has to ask, why prescribe Gaviscon at all, or for that matter, any acid inhibitor? Especially when the side effects of Gaviscon are bloating, constipation, nausea and making the baby feel less hungry because it expands to fill the stomach. Not great when we need our newborns to feed well. All of this causes more discomfort for them at a time of exponential development. Constipation in a small body that is only just beginning to learn how milk/food feels in the digestive tract as it’s processed can cause a lot of unsettled behaviours like reduced sleep, crying, screaming, pedaling legs, arching backwards, not wanting to be put down or be bent (sat) to name a few. Not feeling hungry may also has its consequences on the demand and supply mechanism of breastfeeding and the child’s weight gain over time. It’s also important to be aware that sodium alginate is high in sodium, one dose of Gaviscon potentially contains more than one gram but the recommended daily limit for sodium for newborns to one year olds is 0.4grams.3
Ranitidine
Ranitidine is a H2-blocker that decreases the amount of acid that the parietal cells in the stomach produce. The basis of giving ranitidine to baby’s is the same as gaviscon, that it will reduce the upset from the acid that may move back up the oesophagus, even though, again, acid is not the cause of the majority of upset.
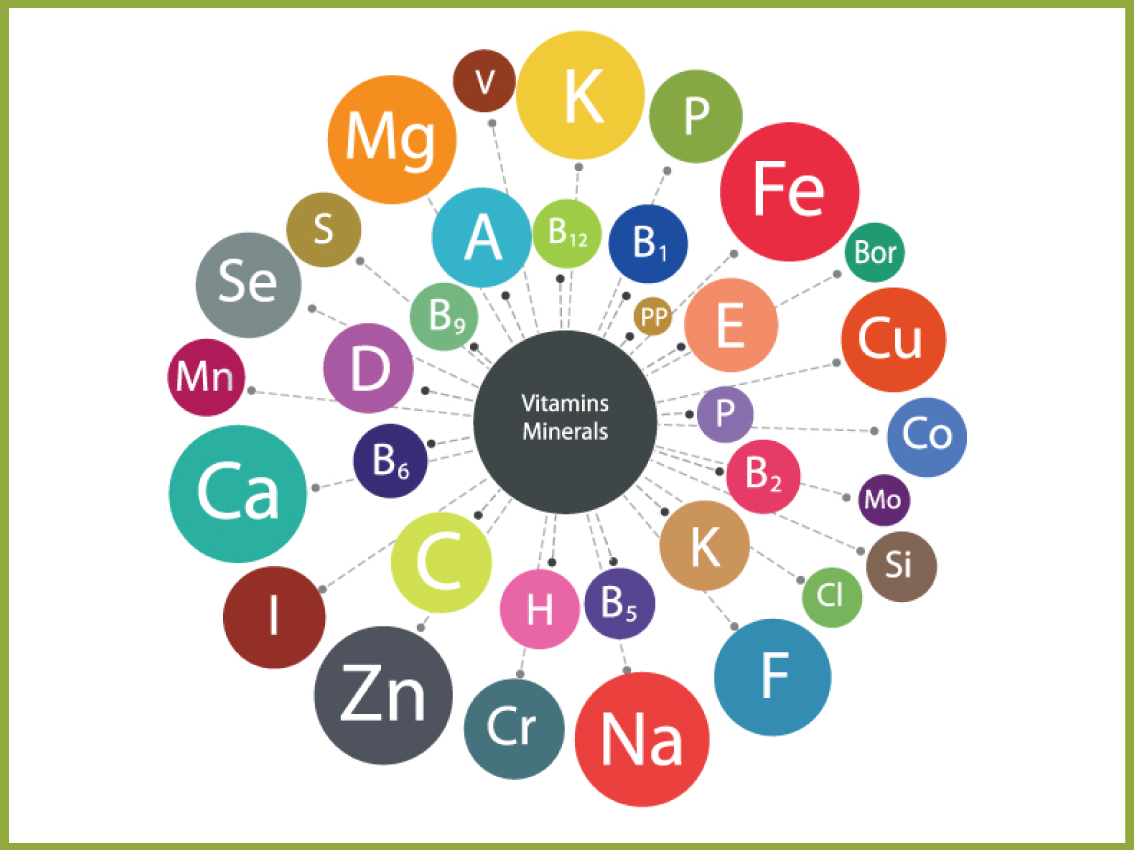
With the reduction of acid that Ranitidine creates, a baby’s digestive function becomes compromised. Hydrochloric acid (HLC) is vital to immunity, keeping invading bacteria and virus at bay. It is a much needed component for a baby’s health as it also helps them breakdown their essential vitamins and minerals so they can be absorbed and used for their mental and physical development. While H2 blockers allow a little absorption to continue because they only reduce acid levels, Proton Pump Inhibitors (outlined below) allow no absorption as they completely stop acid production.
This means our newborns can no longer absorb iron, calcium, magnesium, B12 (essential for brain development and only present in small amounts at birth so vital to receive through their food) and other important nutrients critical for optimum health. Furthermore, there is evidence that acid suppression does nothing to improve these distressing behaviours and that PPI and H2 Blocker therapies are associated with important adverse effects.’4 If you would like to read more about these, non-absorption of nutrients and the FDA regulations around H2 Blockers and Proton Pump Inhibitors feel free to click on the link opposite.
Proton Pump Inhibitors
As mentioned above, PPI’s stop the production of acid in the stomach. The body however knows it needs to produce acid so it automatically begins to make more acid to override the drug. This means, that when these PPI’s and H2 Blockers are weaned, the newborn will experience a backwash of acid, and because they often get worse during this time, the parents believe the drug is working to the child’s advantage so they understandably re administer. Also, because these drugs have been proven to not stop reflux symptoms, the paediatrician will sometimes increase the dose when the parent returns to them letting them know the reflux hasn’t changed that much. They may have calmed slightly because they are feeling the effects of not receiving the nutrients, but this is often short lived as parts of the digestive system struggle with aspects of food and waste they are not meant to. The reflux doesn’t stop either.
Amino acid-based formula
Now because the PPI hasn’t worked and the pediatrician knows that some of the upset your child is now experiencing is because they can’t breakdown their milk or food anymore, they will go onto prescribe an amino-based formula. These formulas are genetically modified and don’t require the digestive system to work at breaking them down. This can often work when baby is only formula fed, but when they are then introduced to solids as an infant, there behaviour can heighten again. At this stage some pediatricians suggest increasing the dose because of the child’s weight.
I have to add here, I am not out to portray pediatricians as awful. They are amazing at what they can do for our children. AMAZING! But like all professions there are good ones, and not so good ones. Those that chase the money and those that will refuse to administer these acid inhibitors to parents because they truly follow best practice for health. Sadly these pediatricians sometimes get a bad rap from parents whom have been told to try the inhibitors by others, but get told no at their appointment. Especially because, until now, there has been little else to offer.
AR formula
AR formula is a rice thickened formula that apparently helps newborns reduce spit up. Marketed as a good choice for reflux, these formulas are not ideal for the digestive system of a newborn, because they simply do not have the enzymes required to fully break down rice in a healthy manner until at least one year of age - and yes that does include baby rice, which I also don't recommend for infant’s.
Some of these formulas use carob bean gum, a natural food additive that comes from the carob seeds of the carob tree. While there are positives reported about carob bean gum it is also important to recognise that it may slow gastric emptying rate, delaying movement of food from the stomach to small intestines. If a baby is on a PPI and being fed often (within 3 ½ hours, so faster than the baby’s digestive system can naturally cope with) this slowing could place extraordinary pressure on the stomach, intestine and bowel.
Also, a study in 2012 showed a “possible association between necrotizing enterocolitis and ingestion of a commercial feed thickener by premature infants.”6 Necrotizing enterocolitis (NEC) is a devastating disease that affects mostly the intestine of premature infants. The wall of the intestine is invaded by bacteria, which causes local infection and inflammation that can ultimately destroy the wall of the bowel (intestine).7
Maple Syrup
Now this is something that I have heard about in the last six months. Because the above formulas taste awful and newborns and infants often refuse them, it is now being suggested that parents add maple syrup to the formula. The adverse effect of this is obviously far too much sugar for one so young, and if fake maple syrup is used, then there are further health consequences. Most imitation syrup is made with corn syrup as the main ingredient. This is processed to form a concentrated fructose syrup. According to a study published in April 2004 in "The American Journal of Clinical Nutrition," consuming high-fructose corn syrup may lead to weight gain and obesity. This may be because fructose is processed differently in your body than other sugars. It does not stimulate insulin secretion and accumulates in your liver, which may cause a fatty liver, interruption of hunger signals and possibly diabetes.7
Healthy remedies for Digestive Overload
- Feed your baby and infant within their digestive capabilities and capacities for their age. You can read more about this here.
- If your child is now on solids and you’d like to know how to do this, please feel free to contact me for a Simplify Solids Consultation.
- Burp baby well after every feed, and I’m talking more than a couple of burps. You can read more about this here and in my BabyCues Book where you can learn what I have named Nature’s Wind Sequence, an innate sequence of trapped wind in the stomach that once known, helps you to release 10-25 burps after each feed in accordance to your child’s age.
- Check your baby, or infant doesn’t have a tongue or lip tie.
- If breastfeeding check your breastfeeding diet - more about this in my book.
- Homeopathic remedies are great when you know what to use. I use a few in particular within my consultations.
- Take your baby to a good osteopath. They can help relax the vagus nerve which connects the brain to the digestive system. Digestive Overload behaviour puts a strain on this.
- Make sure you get some time out of some kind. Even if it’s five minutes to sit outside without anyone needing anything from you.
- Be kind to yourselves too.